Clozapine Comparison
When working with Clozapine comparison, an analysis that pits clozapine against other antipsychotic medicines to help decide the best fit for a patient. Also known as clozapine vs other drugs, it offers a clear picture of strengths, drawbacks, and practical considerations.
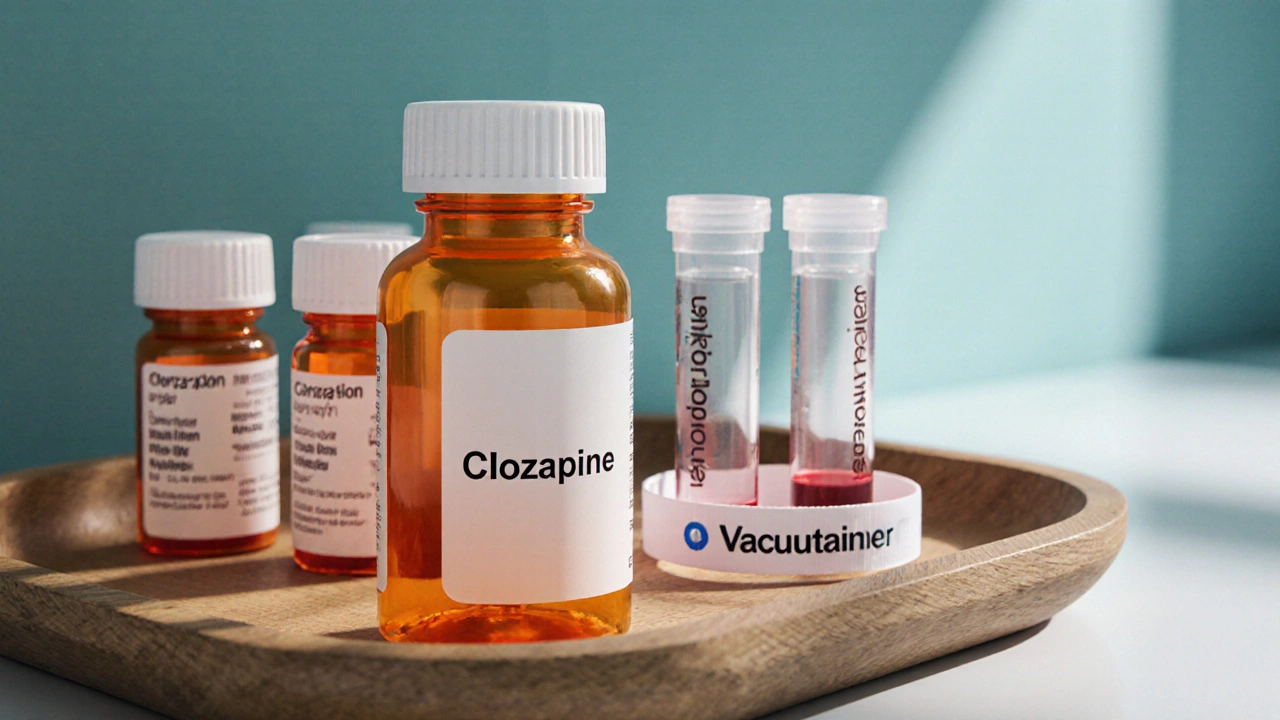
At the heart of any Clozapine comparison lies the drug itself. Clozapine is a second‑generation antipsychotic approved for treatment‑resistant schizophrenia and for reducing suicidal thoughts in patients with psychosis. Its unique receptor profile gives it high efficacy where many other meds fall short, but it also demands regular blood tests because of rare but serious agranulocytosis.
Another big player in the field is Risperdal, the brand name for risperidone. Risperdal is a widely used atypical antipsychotic that targets dopamine and serotonin receptors, offering good symptom control for many patients with schizophrenia. When you place risperidone next to clozapine in a comparison, you immediately see trade‑offs: risperidone is easier to monitor but may not work for those who have failed other treatments.
Both drugs belong to the broader class of antipsychotic medications. These medicines are designed to manage psychotic symptoms such as hallucinations, delusions, and disorganized thinking. The class splits into first‑generation (typical) and second‑generation (atypical) agents, each with its own side‑effect fingerprint. Understanding where clozapine and risperidone fit helps clinicians tailor therapy to a patient’s history.
The disease context matters just as much as the drug choice. Schizophrenia is a chronic mental disorder affecting roughly 1 % of the population, characterized by episodes of psychosis, cognitive decline, and social withdrawal. Effective treatment requires not only symptom reduction but also long‑term maintenance, functional recovery, and quality‑of‑life improvements. A solid clozapine comparison should therefore address how each medication impacts these broader goals.
When you line up efficacy, safety, and cost, a few semantic triples emerge naturally: "Clozapine comparison encompasses efficacy evaluation," "Clozapine comparison requires regular blood monitoring," and "Risperdal influences treatment choice for patients who cannot tolerate intensive monitoring." These links show the logical flow from drug properties to real‑world decision making.
Side‑effect profiles often tip the scales. Clozapine can cause weight gain, metabolic changes, and the dreaded neutropenia, while risperidone may lead to prolactin elevation, extrapyramidal symptoms, or mild sedation. Cost is another axis—clozapine’s monitoring program adds hidden expenses, whereas generic risperidone is usually cheaper and more readily available.
Putting all this together, a practical clozapine comparison helps you answer three key questions: Is the patient truly treatment‑resistant? Can they commit to weekly blood draws? Which side‑effect profile aligns best with their health status? Below you’ll find detailed articles that break down each of these points, compare dosing strategies, review real‑world outcomes, and give tips on navigating insurance and pharmacy hurdles.
Ready to dive deeper? The collection that follows unpacks clozapine versus risperidone, other atypicals, and the latest guidelines—all organized so you can pick the right tool for the right patient without losing track of safety or cost.
Clozaril (Clozapine) vs Other Antipsychotics: A Practical Comparison
A side‑by‑side look at Clozapine (Clozaril) versus other antipsychotics, covering efficacy, safety, monitoring, cost and how to pick the right option for treatment‑resistant schizophrenia.