Variceal Bleeding: Causes, Risks, and What You Need to Know
When you have variceal bleeding, a dangerous rupture of swollen veins in the esophagus or stomach caused by high pressure in the portal vein system. Also known as esophageal variceal hemorrhage, it’s one of the most serious complications of advanced liver disease and requires immediate medical attention. This isn’t a minor bleed—it’s a medical emergency that can kill within hours if not treated fast.
Variceal bleeding doesn’t happen out of nowhere. It’s almost always tied to liver cirrhosis, scarring of the liver that blocks normal blood flow. When the liver gets damaged over time—from alcohol, hepatitis, or fatty liver disease—blood can’t flow through it the way it should. That forces blood to find other paths, often through fragile veins in the esophagus or stomach. These veins stretch, swell, and become esophageal varices, enlarged, thin-walled blood vessels that can burst under pressure. The result? Sudden, massive bleeding that looks like vomiting bright red blood or passing dark, tarry stools.
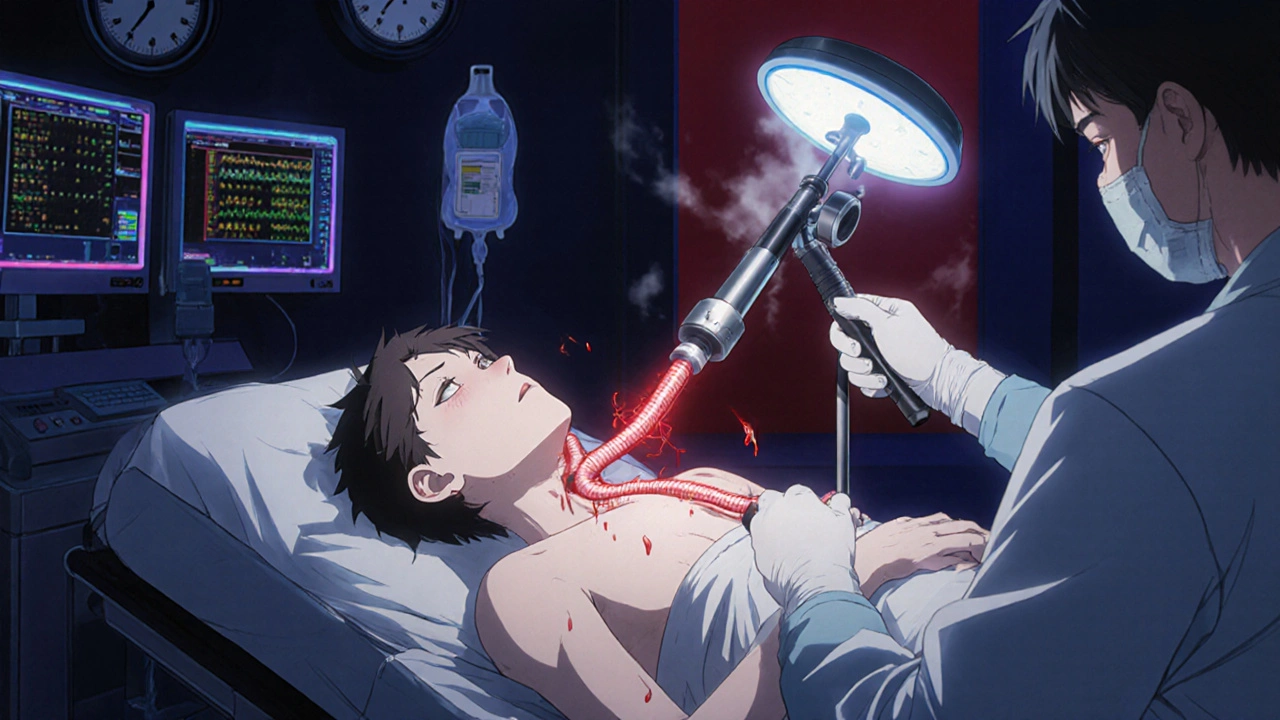
Portal hypertension—the root cause—isn’t just a buzzword. It’s the silent driver behind most cases. It’s what happens when pressure in the portal vein (the main vessel carrying blood from the gut to the liver) climbs above 10 mmHg. At that point, veins start to bulge. People with cirrhosis, especially those who still drink alcohol or haven’t controlled their hepatitis, are at highest risk. But even if you feel fine, if you have advanced liver disease, you could be walking around with unruptured varices. That’s why doctors screen high-risk patients with endoscopy—it’s not optional, it’s lifesaving.
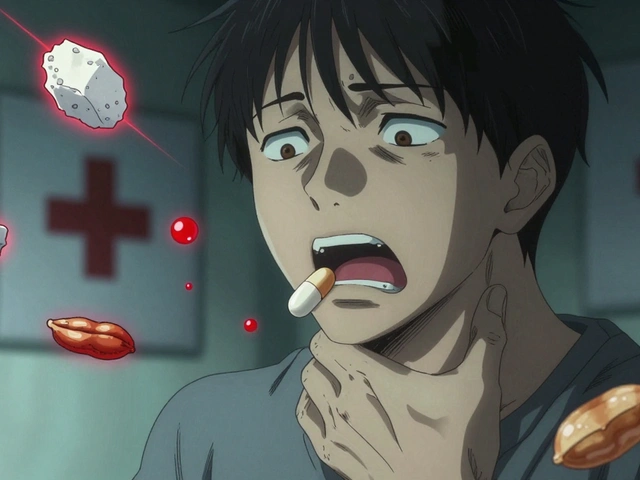
What makes variceal bleeding so dangerous isn’t just the blood loss. It’s what follows. The body goes into shock. The liver can’t clear toxins. Infections like spontaneous bacterial peritonitis often show up right after. And if you’ve had one bleed, your chance of another is over 70% within a year. That’s why treatment isn’t just about stopping the current bleed—it’s about preventing the next one. Medications like beta-blockers (propranolol, nadolol) lower pressure in the portal system. Endoscopic banding seals off the swollen veins. Sometimes, a TIPS procedure (a shunt placed inside the liver) reroutes blood flow entirely.
There’s no sugarcoating this: variceal bleeding is tied to long-term damage. But knowing the signs—vomiting blood, dizziness, rapid heartbeat, black stools—can save your life or someone else’s. If you or a loved one has cirrhosis, don’t wait for symptoms. Ask about screening. Get the right meds. Avoid alcohol. These aren’t just recommendations—they’re your best defense.
Below, you’ll find real-world guides on related conditions like liver health, medication risks, and how to manage chronic diseases that lead to complications like this. No fluff. Just clear, practical info you can use.
Variceal Bleeding: How Banding, Beta-Blockers, and Prevention Save Lives
Variceal bleeding is a life-threatening complication of liver cirrhosis. Learn how endoscopic banding, beta-blockers like carvedilol, and early prevention can stop bleeding, reduce rebleeding, and save lives.