Menstrual Disorders: What They Are and How to Deal With Them
Periods are a normal part of life, but when they’re irregular, too heavy, or painful, they can become a real hassle. That’s what we call menstrual disorders. They affect many people and can signal anything from stress to a health condition that needs treatment. Below you’ll find the most common problems, what to watch for, and simple steps you can take right now.
Common Types of Menstrual Disorders
Irregular periods – Your cycle might be shorter than 21 days, longer than 35 days, or just skip months. Hormone swings, thyroid issues, or weight changes often cause this.
Heavy bleeding (menorrhagia) – If you need to change your pad or tampon every hour, lose clots larger than a quarter, or feel dizzy, you could be dealing with heavy bleeding. Fibroids, polyps, or clotting problems can be behind it.
Painful cramps (dysmenorrhea) – Cramping that makes it hard to work or sleep isn’t normal. Endometriosis or pelvic inflammation can make the pain worse than a typical period.
Premenstrual syndrome (PMS) – Mood swings, bloating, breast tenderness, and fatigue that show up a week before your period are classic PMS signs. For some, the symptoms are severe enough to affect daily life.
Absence of periods (amenorrhea) – Not getting a period for three months or more, without being pregnant, is a red flag. It can point to hormonal imbalance, high stress, or an underlying medical issue.
How to Manage and Seek Help
First, keep a simple period tracker. Write down the start date, flow level (light, medium, heavy), and any symptoms you notice. A few weeks of notes give your doctor a clear picture.
If you notice any of the following, book an appointment: bleeding that soaks through a pad in an hour, periods shorter than two days, severe pain that doesn’t improve with over‑the‑counter pain relievers, or sudden missed periods. Prompt medical attention can rule out serious causes.
Lifestyle tweaks can make a big difference. Regular exercise, balanced meals, and enough sleep help keep hormones steady. Cutting back on caffeine and alcohol may also reduce cramping and mood swings.
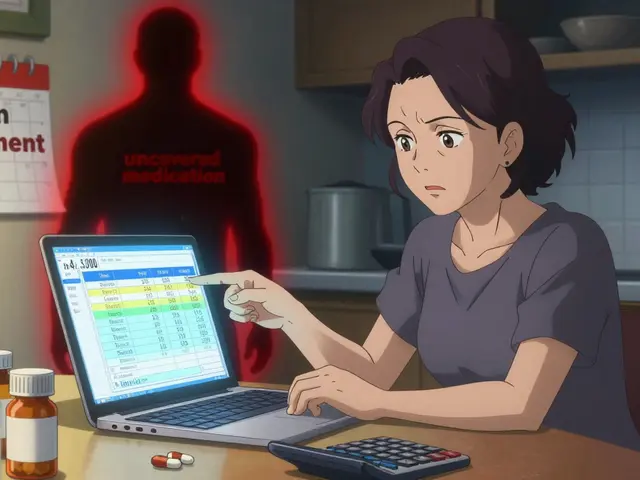
Over‑the‑counter options like ibuprofen or naproxen work well for mild pain and heavy flow. If those don’t help, your doctor might suggest hormonal birth control, a levonorgestrel IUD, or prescription medications that target specific conditions.
Don’t forget mental health. Stress can mess with your cycle, so try relaxation techniques—deep breathing, short walks, or simple yoga poses. Talking to a counselor or joining a support group can also ease the emotional side of PMS.
When you see a specialist, be ready to discuss your tracker, any family history of menstrual issues, and current medications or supplements. Tests may include blood work, ultrasound, or a pap smear, depending on what’s needed.
Remember, menstrual disorders are treatable. With the right info, a bit of tracking, and help from a healthcare professional, you can get your cycle back on track and feel a lot better day to day.
Danazol vs Alternatives: A Comprehensive Drug Comparison
A detailed comparison of Danazol with key alternatives, covering mechanisms, side‑effects, costs, and when each option is best suited for endometriosis and menstrual issues.