What Exactly Are Pharmacodynamic Drug Interactions?
When two drugs are taken together, they don’t just sit in your body like strangers on a bus. Sometimes, they talk to each other-at the very spot where they do their job. This is what pharmacodynamic drug interactions are: changes in how a drug works because another drug is messing with its target, not its amount in your blood.
Think of it like this: if you take two painkillers and feel way more relief than expected, that’s not because there’s more drug in your system. It’s because both drugs are working together at the same receptors. Or if you take a blood pressure med and then an NSAID like ibuprofen, and your blood pressure doesn’t drop like it should-that’s not because the blood pressure drug got metabolized faster. It’s because ibuprofen is blocking a pathway your blood pressure drug needs to work.
This is different from pharmacokinetic interactions, where one drug changes how your body absorbs, breaks down, or gets rid of another. Pharmacodynamic interactions? They’re all about what happens at the receptor level. The drug concentration stays the same. But the effect? That’s where things get unpredictable.
Three Ways Drugs Can Team Up-or Fight
Pharmacodynamic interactions fall into three clear buckets: synergistic, additive, and antagonistic. Each has real-world consequences.
- Synergistic: The combined effect is stronger than the sum of the parts. Think of trimethoprim and sulfamethoxazole (Bactrim). Together, they block two steps in a bacteria’s folic acid production. Alone, each drug needs a high dose. Together? They work at 75% lower doses. That’s synergy in action.
- Additive: The total effect equals the sum of each drug’s effect. Take two sedatives, like benzodiazepines and alcohol. Each makes you drowsy. Together? You’re twice as drowsy. No surprise, no magic-just added up.
- Antagonistic: One drug blocks or reduces the effect of another. This is where things get dangerous. Beta-blockers like propranolol can completely shut down the bronchodilating effect of albuterol in asthma patients. Why? They both fight for the same beta-2 receptors. Propranolol wins because it binds tighter. The result? A patient can’t breathe, even though they took their rescue inhaler.
The Real Danger: When Drugs Cancel Each Other Out
Some of the most life-threatening interactions happen when drugs directly oppose each other. Take opioid painkillers like morphine and opioid blockers like naloxone. If someone is dependent on opioids and gets naloxone-say, for a suspected overdose-the result isn’t just reduced pain relief. It’s full-blown withdrawal: sweating, vomiting, seizures, even cardiac arrest.
Another terrifying combo: SSRIs like sertraline with MAOIs like phenelzine. Together, they cause serotonin syndrome. Your brain gets flooded with serotonin. Symptoms? High fever, muscle rigidity, confusion, irregular heartbeat. A 2021 meta-analysis found this combination increases serotonin syndrome risk by 24-fold. And it doesn’t take much-sometimes just one extra dose of an SSRI on top of an MAOI is enough.
Even common drugs can cause trouble. NSAIDs like ibuprofen or naproxen reduce the effectiveness of ACE inhibitors (like lisinopril) and diuretics. How? They block prostaglandins, which help keep blood flow to the kidneys steady. Without them, kidney blood flow drops by about 25%. That means blood pressure doesn’t drop, and fluid builds up. A 2019 NIH study of 347 hypertensive patients showed this interaction happens more often than doctors realize.
Why These Interactions Are Hard to Spot
Pharmacodynamic interactions are sneaky because they don’t show up in blood tests. Your doctor can check your lithium level. They can see if your statin is too high. But they can’t measure how well your beta-blocker is working against your inhaler. You just feel worse.
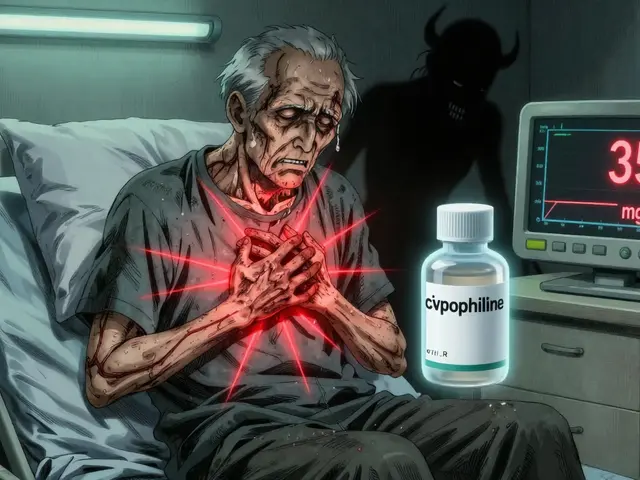
And it’s not just about the drugs themselves. It’s about the person. Elderly patients are the most at risk. On average, they take 4.8 prescription medications. Many of those drugs affect the central nervous system-sleep aids, antidepressants, pain meds, antipsychotics. Combine them, and you’ve got a recipe for falls, confusion, or worse.
A 2022 survey of over 1,200 physicians found that 63% ran into a dangerous pharmacodynamic interaction at least once a month. The top culprits? Anticoagulants with antiplatelets (like warfarin and aspirin) and CNS depressants stacked together. One pharmacist on Reddit described a near-fatal case where linezolid (an antibiotic) and sertraline triggered serotonin syndrome in an elderly woman. She ended up in ICU for 72 hours.
When the Interaction Actually Helps
Not all pharmacodynamic interactions are bad. Medicine uses them on purpose.
The combo of levodopa and carbidopa is a classic example. Levodopa crosses the blood-brain barrier to become dopamine. But it gets broken down too fast by enzymes in the gut. Carbidopa blocks those enzymes-so more levodopa reaches the brain. The result? Better Parkinson’s control with lower doses and fewer side effects.
Another example: low-dose naltrexone (LDN) with antidepressants. A 2021 study of 142 patients with treatment-resistant depression found that adding LDN boosted response rates from 42% to 68%. The theory? Naltrexone briefly blocks opioid receptors, triggering the body to produce more endorphins-natural mood lifters. It’s not widely used yet, but it shows how understanding these interactions can unlock new treatments.
Who’s Most at Risk-and How to Stay Safe
People taking drugs with a narrow therapeutic index are in the danger zone. That means the difference between a helpful dose and a toxic one is tiny. Think warfarin, digoxin, lithium, or thyroid meds. A small shift in effect can mean hospitalization.
According to NIH data, 83% of life-threatening pharmacodynamic interactions involved at least one drug with a therapeutic index below 3.0. That’s why it’s not enough to just check a drug interaction app. You need to know the drugs you’re prescribing-or taking.
Here’s what you can do:
- Know your high-risk combos: NSAIDs + ACE inhibitors, SSRIs + MAOIs, beta-blockers + beta-agonists, opioids + naloxone.
- Ask about all meds: Including OTC drugs, supplements, and alcohol. Many people don’t think ibuprofen or St. John’s wort counts.
- Watch for symptoms: If you’re on multiple meds and suddenly feel dizzy, confused, short of breath, or unusually tired-don’t brush it off.
- Use pharmacist reviews: A 2021 review in BMJ found pharmacist-led medication checks reduced adverse events from these interactions by 58% in older adults.
The Future: Better Tools, Better Outcomes
Technology is catching up. Clinical decision support systems in hospitals now flag potential interactions, but they still miss about 22% of serious ones. Why? Many systems only look at pharmacokinetic risks. They don’t model receptor competition or physiological interference well.
But new tools are coming. The NIH is funding over $28 million in research to build machine learning models that predict interactions before they happen. One UCSF team developed an algorithm that predicts serotonin syndrome risk with 89% accuracy-based on a patient’s full drug list, age, kidney function, and genetic markers.
In the UK, the NHS is piloting real-time alerts in electronic health records. If a doctor tries to prescribe an SSRI to someone already on an MAOI, the system doesn’t just warn-it blocks the order and suggests alternatives.
And it’s not just about tech. Medical schools are finally teaching pharmacodynamics with real cases, not just theory. The CICM Primary exams in Australia and the UK now require candidates to name five specific examples of each interaction type. That’s progress.
Bottom Line: It’s Not About the Dose-It’s About the Effect
Pharmacodynamic interactions aren’t rare. They’re common. And they’re dangerous because they’re invisible. You can’t see them on a lab report. You can’t measure them with a machine. You have to understand how drugs behave at the cellular level-and how your body responds.
Whether you’re a patient taking five meds or a clinician writing prescriptions, the message is the same: Don’t assume drugs play nice together. Even if they’re prescribed by different doctors. Even if they’re over-the-counter. Even if you’ve taken them for years.
The safest approach? Always ask: What’s this drug trying to do? And what’s the other one doing to stop it-or make it worse? That’s how you avoid the hidden dangers-and sometimes, unlock the hidden benefits.
What’s the difference between pharmacodynamic and pharmacokinetic drug interactions?
Pharmacokinetic interactions change how your body handles a drug-like how fast it’s absorbed, broken down, or cleared. Pharmacodynamic interactions change how the drug works at its target site, even if its concentration stays the same. For example, an antibiotic might be metabolized faster by another drug (pharmacokinetic), or a beta-blocker might block an asthma inhaler from working (pharmacodynamic).
Can over-the-counter drugs cause pharmacodynamic interactions?
Yes. Common OTC drugs like ibuprofen, naproxen, and even antihistamines can interfere with prescription meds. Ibuprofen reduces the effect of blood pressure drugs. Diphenhydramine (Benadryl) can add to drowsiness from antidepressants or sleep aids. Always check OTC meds with your pharmacist.
Why are elderly patients more at risk for these interactions?
Older adults often take multiple medications-on average, 4.8 prescriptions. Many of these affect the brain or heart, and their bodies process drugs differently. Kidney and liver function decline with age, and receptors become more sensitive. Even small changes in drug effect can lead to falls, confusion, or organ damage.
Are there any safe combinations of drugs that work better together?
Yes. Trimethoprim and sulfamethoxazole work better together than alone. Levodopa and carbidopa improve Parkinson’s symptoms with fewer side effects. Low-dose naltrexone combined with antidepressants has shown promise for treatment-resistant depression. These are intentional, evidence-based synergies-not accidents.
How can I check for drug interactions myself?
Use reliable databases like the University of Liverpool’s HIV Drug Interactions Checker (even if you don’t have HIV-it’s one of the most comprehensive), or apps like Micromedex or Lexicomp. But don’t rely only on apps. Talk to your pharmacist. They’re trained to spot subtle interactions that algorithms miss.
What should I do if I think I’m having a drug interaction?
Don’t stop your meds suddenly-some can cause dangerous withdrawal. Call your doctor or pharmacist right away. Write down your symptoms, when they started, and all the drugs you’re taking-including vitamins and supplements. Bring this list to your appointment. Early recognition can prevent hospitalization.




Shawn Peck January 30, 2026
Look, I don't need a 10-page essay to know this: mixing drugs is dangerous. I saw a guy on the news take ibuprofen with his blood pressure med and end up in the ER. Simple. Don't mix. Ask your pharmacist. Done.
Beth Beltway January 31, 2026
This post is technically correct but completely misses the point. Pharmacodynamic interactions aren't even the biggest problem - it's the fact that 70% of prescribers can't name the top five high-risk combos without looking them up. And don't get me started on how EHRs still treat all interactions as binary yes/no flags when reality is a fucking gradient. Also, why is no one talking about polypharmacy in geriatrics being a systemic failure of healthcare design, not just a 'patient issue'?
Kimberly Reker February 2, 2026
I work in a pharmacy and I see this every day. Elderly patients come in with 8 different meds from 4 different doctors. One lady was on sertraline, naproxen, lisinopril, and melatonin. She kept falling. We caught the NSAID + ACE inhibitor interaction. She was so relieved. Just because something is 'over-the-counter' doesn't mean it's safe with your other stuff. Always bring your whole list - including that gummy vitamin you think doesn't count.
Jason Xin February 3, 2026
Wow. Someone actually wrote a post that doesn't sound like it was generated by a chatbot trying to pass a med school exam. Respect. I used to think 'drug interactions' meant 'don't mix alcohol and X.' Turns out it's way creepier - like your beta-blocker quietly stealing the spotlight from your inhaler. Scary stuff. And yeah, the serotonin syndrome thing? That's not a myth. I lost a friend to that. No warning. Just... gone.
Kathleen Riley February 3, 2026
The ontological underpinnings of pharmacodynamic interaction necessitate a re-evaluation of the Cartesian dichotomy between agent and effect. When two pharmacophores compete for receptor occupancy, we are not merely observing biochemical interference - we are witnessing the collapse of therapeutic intentionality into emergent physiological chaos. The body, as a self-regulating autopoietic system, becomes a contested terrain where molecular sovereignty is violently contested. This is not pharmacology. This is bio-political warfare.
Sazzy De February 4, 2026
My grandma takes 6 pills a day and swears she's fine but she's always dizzy. I told her to get her meds reviewed. She said 'but the doctor said it's fine' and I was like... honey the doctor didn't even know you were taking that turmeric supplement
Kelly Weinhold February 4, 2026
I just want to say - this is so important and I'm so glad someone took the time to explain it clearly. I used to think if a drug was 'prescribed' it was automatically safe. But after my mom had that bad reaction to her blood pressure med and ibuprofen, I started asking questions. Now I bring a list to every appointment. It feels weird at first but your pharmacist will thank you. Seriously. They're the real MVPs of healthcare.
Sheila Garfield February 6, 2026
I'm a nurse and I've seen this too many times. The worst part? Patients feel guilty when something goes wrong. Like it's their fault for taking the meds. But it's not. It's a system failure. We need better communication between providers. And maybe a universal med list that follows you like your credit score. Just saying.
Amy Insalaco February 7, 2026
While the post presents a superficially coherent taxonomy of pharmacodynamic interactions, it fundamentally misrepresents the epistemological hierarchy of clinical decision-making by privileging mechanistic reductionism over systems biology. The receptor-centric model ignores the pleiotropic modulation of signaling cascades, allosteric crosstalk, and transcriptional feedback loops that modulate downstream phenotypes. Moreover, the reliance on pairwise interaction databases is a relic of 20th-century pharmacology. Modern polypharmacy requires network pharmacology models that account for emergent dynamics - something no EHR or app currently possesses. Until then, we are all just guessing.
Sarah Blevins February 7, 2026
The 24-fold increase in serotonin syndrome risk with SSRI/MAOI co-administration is statistically significant but lacks context regarding population prevalence. The absolute risk remains low. Furthermore, the NIH study cited on NSAID/ACE inhibitor interaction was observational with potential confounding by indication. Correlation ≠ causation. This post reads like alarmist clinical propaganda.
Donna Fleetwood February 8, 2026
I used to think drug interactions were just for doctors. Then I got on 4 meds after my surgery and started feeling weird. I wrote down everything I took - even the herbal tea - and showed it to my pharmacist. She caught that my sleep aid was making my antidepressant less effective. We switched one thing and I felt like myself again. You don't need to be a genius to save your own life. Just be organized.
Carolyn Whitehead February 9, 2026
My dad is 78 and takes 7 meds. He doesn't even remember all of them. I made him a color coded chart with pictures. He still forgets sometimes but now he knows to call me if he feels off. It's not glamorous but it keeps him safe. Small steps matter
Diksha Srivastava February 10, 2026
In India, people buy antibiotics and painkillers without prescriptions. I've seen friends mix ibuprofen with blood pressure pills because they felt 'a little dizzy.' No one tells them this stuff. We need community education - not just hospital alerts. Pharmacists in small towns need training too.
Melissa Cogswell February 12, 2026
I'm a med student and this was our first real case study. We had to analyze a patient on warfarin, aspirin, and fluoxetine. The interaction wasn't obvious until we mapped out the receptor effects. It clicked for me then - drugs aren't just chemicals. They're actors on a stage. One changes the script, and everyone else has to improvise.
Adarsh Uttral February 12, 2026
i read this and thought wow i never knew ibuprofen could mess with my dad's heart med. now i check his meds every week. also he started taking fish oil and i was like wait is that safe? turned out it is but i asked a pharmacist first. best thing ever