ALT Elevation Statins: What It Means and What to Do
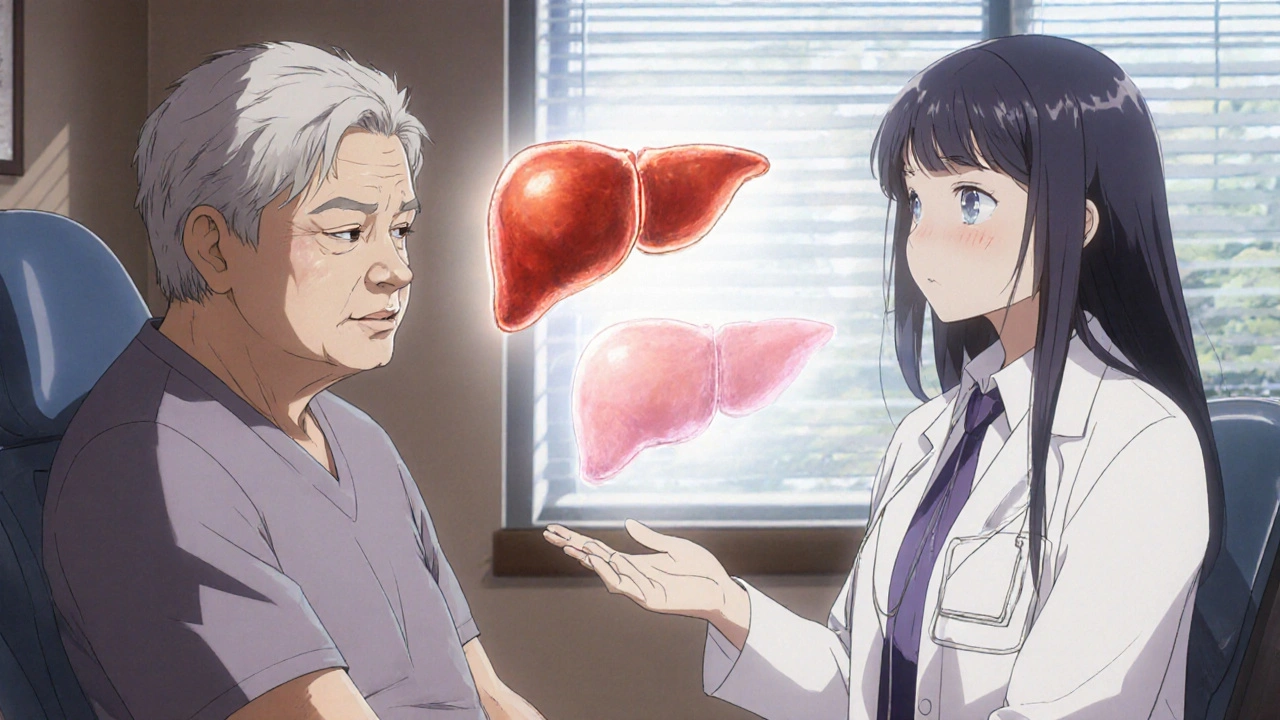
When you take a statin, a class of cholesterol-lowering drugs used to reduce heart attack and stroke risk. Also known as HMG-CoA reductase inhibitors, they’re among the most prescribed medications in the U.S. Many people on statins get a blood test back showing elevated ALT, alanine aminotransferase, an enzyme found mostly in the liver that signals stress or damage when levels rise. It sounds scary—liver damage? But here’s the truth: most of the time, it’s not. ALT spikes on statins happen in up to 3% of users, and in over 90% of those cases, the levels go back to normal on their own, even if you keep taking the drug.
ALT elevation doesn’t mean you have liver disease. It just means your liver cells are releasing a bit more enzyme than usual—maybe because the statin is making them work harder to process the drug. Think of it like your muscles getting sore after a new workout. It’s a signal, not a breakdown. What matters more is how high the ALT is, whether other liver enzymes like AST are also up, and if you have symptoms like yellow skin, dark urine, or constant fatigue. If your ALT is under 3 times the upper limit of normal and you feel fine, your doctor will likely just monitor it. No need to panic. Many patients stay on statins for years with mild ALT changes and no harm done.
But if your ALT is really high—or if you start feeling unwell—your doctor might switch you to a different statin. Not all statins affect the liver the same way. Atorvastatin and rosuvastatin tend to be gentler on liver enzymes than simvastatin or fluvastatin. Sometimes, lowering the dose helps. Other times, switching to a non-statin option like ezetimibe or a PCSK9 inhibitor makes sense. The goal isn’t to avoid statins at all costs—it’s to keep your heart protected while keeping your liver safe. That’s why regular blood tests are part of the deal when you’re on these meds.
You’ll also see posts here about how other drugs, like sertraline or ribavirin, can affect liver enzymes too. But statins are different because they’re taken long-term by millions of people, many of whom have no other liver issues. The key is context: your age, weight, alcohol use, other meds, and existing conditions like diabetes or fatty liver all play a role. If you’re overweight or have metabolic syndrome, even a small ALT rise might mean your liver is already under strain—and statins might be helping more than hurting.
What you won’t find here are scare stories about statins destroying your liver. You’ll find real, practical advice from people who’ve been there: how to talk to your doctor, what bloodwork to ask for, when to push back on stopping your meds, and how to support your liver naturally—without skipping your heart protection. The posts below cover everything from comparing statin brands to understanding liver enzyme patterns, managing side effects, and knowing when to switch. This isn’t about avoiding statins. It’s about using them wisely.
Statin‑Induced Liver Enzyme Elevation: What You Need to Know
Learn why statins may mildly raise ALT/AST, how common serious liver injury is, and what monitoring and management steps keep you on therapy safely.