Statin Safety: What You Need to Know About Side Effects, Risks, and Real-World Use
When doctors prescribe statins, a class of drugs used to lower LDL cholesterol and reduce heart attack risk. Also known as HMG-CoA reductase inhibitors, they're among the most prescribed medications in the U.S. because they work—for most people. But statin safety isn't just about whether they lower cholesterol. It’s about whether they’re safe for you, long-term.
Many people worry about muscle pain, fatigue, or liver issues after starting a statin. These aren’t just rumors. Studies show about 1 in 10 people report muscle aches, and for a small number, it’s bad enough to stop the drug. But here’s what most don’t realize: if you’re taking a statin because you’ve had a heart attack or have diabetes, the risk of another cardiac event without it is far higher than the chance of serious side effects. That’s the trade-off. And it’s not just about muscles. Statins can slightly raise blood sugar, which matters if you’re prediabetic. They’re not harmless, but they’re not the danger some online posts make them out to be either.
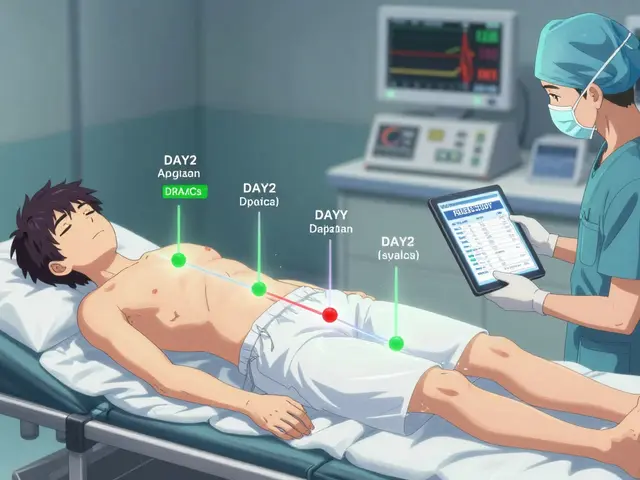
What you won’t hear from your doctor often is that statin side effects, range from mild muscle discomfort to rare but serious conditions like rhabdomyolysis. Also known as muscle breakdown, it’s extremely uncommon—less than 1 in 10,000 users—but it can damage kidneys if ignored. That’s why tracking symptoms matters. If your legs feel heavy after starting a statin, don’t assume it’s just aging. Talk to your doctor. Maybe switching from atorvastatin to rosuvastatin helps. Or lowering the dose. Or trying a different type of cholesterol-lowering drug altogether. statin alternatives, include ezetimibe, PCSK9 inhibitors, and even high-dose fish oil in some cases. Also known as non-statin lipid-lowering therapies, they’re not first-line—but they’re options when statins don’t fit. You’re not stuck with one drug just because it was prescribed first.
And here’s something else: statin safety isn’t just about the drug. It’s about how you live. People who take statins and also walk daily, eat less processed food, and sleep well often need lower doses—or sometimes none at all. The drug isn’t a magic bullet. It’s a tool. The real question isn’t "Should I take a statin?" It’s "What’s my actual risk, and what’s the best plan for me?" That’s what the posts below cover: real stories, real data, and real choices people made after learning the full picture. You’ll find what works, what doesn’t, and what no one told you about statins and your body.
Grapefruit and Statins: What You Need to Know About Dangerous Interactions
Grapefruit can dangerously increase statin levels in your blood, raising the risk of muscle damage and kidney failure. Learn which statins are affected, how to stay safe, and what alternatives exist.